
Build vs. Buy: The True Cost of In-House RBT® Training Programs
For many ABA organizations, the decision to build or buy an RBT® training program seems straightforward until turnover, onboarding inefficiencies, and inconsistent training quality begin eroding margins and clinical outcomes. At that point, what looked like the “cheapest” option quickly becomes the most expensive.
I’ve spent years working with ABA organizations of all sizes, and one theme is remarkably consistent: leaders often underestimate the hidden drivers of cost inside their training ecosystems. As a result, they miss some of the greatest opportunities to improve retention, ensure clinical quality, and increase operational efficiency.
This blog highlights the most common pitfalls I see in in-house RBT training programs and offers a framework leaders can use when evaluating whether to build, buy, or redesign their approach.
Hidden Costs: Turnover Makes “Cheap” Training Very Expensive
When organizations consider training costs, they often focus on the price of the course itself. But many off-the-shelf RBT trainings only cover the minimum requirements needed to sit for the exam. Everything else, clinical best practices, documentation expectations, and company-specific procedures, must be taught separately.
Supplemental training often requires additional shadowing sessions, additional content development, or live instruction from senior staff. Those hours are expensive, and these costs scale quickly with technician volume.
Layered on top of that is a universal issue in our field: turnover at the BT level. The cost of an RBT training license is minimal compared to the full operational cost of replacing a technician. Recruiting, HR processing, onboarding time, and background checks can easily approach, or exceed, the salary of the person being replaced.
That’s why I emphasize designing training environments where people feel competent and confident from the start. When people feel equipped for the role, they are more likely to stay, and even modest improvements in early retention can create substantial organizational savings.
Compliance Training Alone Increases Burnout and Early Attrition
One of the most significant gaps I see across ABA organizations is the divide between training to pass an exam and training to perform in real sessions.
 This disconnect exists across all clinical levels, not just RBTs. The challenge isn’t simply that conceptual training differs from practice. It’s the juxtaposition between a clinician’s training experience and the reality of clinical work. That mismatch can be jarring, and for new clinicians, it often contributes to stress, burnout, and early attrition.
This disconnect exists across all clinical levels, not just RBTs. The challenge isn’t simply that conceptual training differs from practice. It’s the juxtaposition between a clinician’s training experience and the reality of clinical work. That mismatch can be jarring, and for new clinicians, it often contributes to stress, burnout, and early attrition.
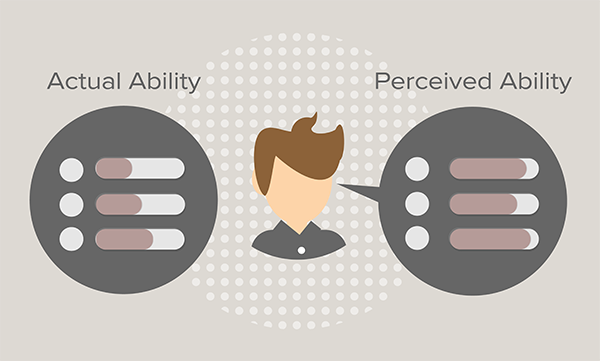
Reading about procedures is fundamentally different from seeing them implemented. Without opportunities to observe nuanced application, practice critical skills, and receive feedback, new staff may develop confidence without competence, a pattern reflected in the Dunning-Kruger effect.
Preparing people for the realities of practice requires training that builds both conceptual understanding and real-world fluency.
Training Variability Across Regions Isn’t a People Problem
When organizations struggle with inconsistent training outcomes across regions or service lines, the cause is usually systemic, either logistical or programmatic.
Logistically, different instructors, environments, or schedules can create drift. Programmatically, if critical components of the training aren’t consistently implemented across trainers, outcomes naturally vary, even when the content is the same.
One thing I’ve seen make a meaningful difference is designing training specifically for the intended audience and ensuring that every learner experiences the critical features of the program and every trainer implements those features with fidelity. When these elements are standardized, organizations see reduced variability across locations and more predictable performance outcomes.
Better Onboarding Improves Retention by Reducing Discomfort on Day One
 We don’t have a single determinant of RBT turnover, but we do know the drivers that matter: training quality, perceived supervisory support, clarity of expectations, and opportunities for professional growth.
We don’t have a single determinant of RBT turnover, but we do know the drivers that matter: training quality, perceived supervisory support, clarity of expectations, and opportunities for professional growth.
Among these, training quality is one of the areas that organizations can most easily influence. If staff begin their role feeling unsure, unprepared, or uncomfortable, they are more likely to leave early. And when people repeatedly encounter aversive conditions, the natural response is to escape the situation, often by leaving the organization entirely.
Training that builds competence early reduces that discomfort. It replaces uncertainty with fluency, providing a foundation for success. When technicians start strong, retention improves.
What Leaders Should Ask Before Choosing to Build or Buy
When leaders weigh the decision to build an internal training program or invest in a professionally designed solution, the right questions determine the right path:
- Does this training reflect our culture and the realities of our practice?
Training should model the performance expectations, values, and workflows that define your organization, not generic content disconnected from daily operations. - Who is this training designed for?
Most RBTs today are members of Gen Z. Long, static, lecture-heavy training formats are mismatched to how this generation learns. Engagement matters for outcomes. - Is this training meant only to meet a compliance requirement, or is it designed to change performance?
Programs built solely for compliance rarely produce fluent, confident, independent practitioners. - Does our approach make new team members feel like part of the team?
Most leaders will say they value each team member. However, if your onboarding consists of handing someone a laptop and asking them to work alone for 40 hours, there’s a disconnect between what you say you value and what your training signals.
Organizations that answer these questions clearly are far better positioned to create scalable, sustainable programs that support clinical quality and workforce stability.
There Is an Alternative to the Status Quo
Many ABA organizations feel locked into a cycle of high turnover, inconsistent training outcomes, and escalating onboarding costs. But it doesn’t have to stay that way.
Thoughtfully designed training, whether built in-house or purchased, can stabilize your workforce, reduce hidden costs, and create more predictable, higher-quality performance across your organization. There is a better way, and it starts with understanding what your training process is truly costing you today.
